Available treatments
There are many products available for the treatment of acne, many of which are without any scientifically proven effects. Generally speaking, successful treatments show little improvement within the first two weeks, instead taking a period of approximately three months to improve and start flattening out. Many treatments that promise big improvements within two weeks are likely to be largely disappointing. However, short bursts of cortisone can give very quick results, and other treatments can rapidly improve some active spots, but usually not all active spots.
Modes of improvement are not necessarily fully understood but in general treatments are believed to work in at least 4 different ways (with many of the best treatments providing multiple simultaneous effects):
- normalising shedding into the pore to prevent blockage
- killing Propionibacterium acnes
- anti-inflammatory effects
- hormonal manipulation
A combination of treatments can greatly reduce the amount and severity of acne in many cases. Those treatments that are most effective tend to have greater potential for side effects and need a greater degree of monitoring, so a step-wise approach is often taken. Many people consult with doctors when deciding which treatments to use, especially when considering using any treatments in combination. There are a number of treatments that have been proven effective:
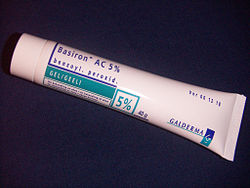
Topical bactericidals
Widely available OTC bactericidal products containing benzoyl peroxide may be used in mild to moderate acne. The gel or cream containing benzoyl peroxide is rubbed, twice daily, into the pores over the affected region. Bar soaps or washes may also be used and vary from 2 to 10% in strength. In addition to its therapeutic effect as a keratolytic (a chemical that dissolves the keratin plugging the pores) benzoyl peroxide also prevents new lesions by killing P. acnes. In one study, roughly 70% of participants using a 10% benzoyl peroxide solution experienced a reduction in acne lesions after 6 weeks.[46] Unlike antibiotics, benzoyl peroxide has the advantage of being a strong oxidizer (essentially a mild bleach) and thus does not appear to generate bacterial resistance. However, it routinely causes dryness, local irritation and redness. A sensible regimen may include the daily use of low-concentration (2.5%) benzoyl peroxide preparations, combined with suitable non-comedogenic moisturisers to help avoid overdrying the skin.
Care must be taken when using benzoyl peroxide, as it can very easily bleach any fabric or hair it comes in contact with.
Other antibacterials that have been used include triclosan, or chlorhexidine gluconate. Though these treatments are often less effective, they also have fewer side-effects.
Prescription-strength benzoyl peroxide preparations do not necessarily differ with regard to the maximum concentration of the active ingredient (10%), but the drug is made available dissolved in a vehicle that more deeply penetrates the pores of the skin.
Topical antibiotics
Externally applied antibiotics such as erythromycin, clindamycin, stievamycin, or tetracycline kill the bacteria that are harbored in the blocked follicles. While topical use of antibiotics is equally as effective as oral use, this method avoids possible side effects including upset stomach and drug interactions (e.g. it will not affect use of the oral contraceptive pill), but may prove awkward to apply over larger areas than just the face alone.
Oral antibiotics
Oral antibiotics used to treat acne include erythromycin or one of the tetracycline antibioticstetracycline, the better absorbed oxytetracycline, or one of the once daily doxycycline, minocycline, or lymecycline). Trimethoprim is also sometimes used (off-label use in UK). However, reducing the P. acnes bacteria will not, in itself, do anything to reduce the oil secretion and abnormal cell behaviour that is the initial cause of the blocked follicles. Additionally the antibiotics are becoming less and less useful as resistant P. acnes are becoming more common. Acne will generally reappear quite soon after the end of treatment—days later in the case of topical applications, and weeks later in the case of oral antibiotics. Furthermore side effects of tetracycline antibiotics can include yellowing of the teeth and an imbalance of gut flora, so are only recommended after topical products have been ruled out. (
It has been found that sub-antimicrobial doses of antibiotics such as minocycline also improve acne. It is believed that minocycline's anti-inflammatory effect also prevents acne.
Hormonal treatments
In females, acne can be improved with hormonal treatments. The common combined oestrogen/progestogen methods of hormonal contraception have some effect, but the antiandrogen, Cyproterone, in combination with an oestrogen (Diane 35) is particularly effective at reducing androgenic hormone levels. Diane-35 is not available in the USA, but a newer oral contraceptive containing the progestin drospirenone is now available with fewer side effects than Diane 35 / Dianette. Both can be used where blood tests show abnormally high levels of androgens, but are effective even when this is not the case. Along with this, treatment with low dose spironolactone can have anti-androgenetic properties, especially in patients with polycystic ovarian syndrome.
If a pimple is large and/or does not seem to be affected by other treatments, a dermatologist may administer an injection of cortisone directly into it, which will usually reduce redness and inflammation almost immediately. This has the effect of flattening the pimple, thereby making it easier to cover up with makeup, and can also aid in the healing process. Side effects are minimal, but may include a temporary whitening of the skin around the injection point; and occasionally a small depression forms, which may persist, although often fills eventually. This method also carries a much smaller risk of scarring than surgical removal.
Topical retinoids
A group of medications for normalizing the follicle cell lifecycle are topical retinoids such as tretinoin (brand name Retin-A), adapalene (brand name Differin), and tazarotene (brand name Tazorac). Like isotretinoin, they are related to vitamin A, but they are administered as topicals and generally have much milder side effects. They can, however, cause significant irritation of the skin. The retinoids appear to influence the cell creation and death lifecycle of cells in the follicle lining. This helps prevent the hyperkeratinization of these cells that can create a blockage. Retinol, a form of vitamin A, has similar but milder effects and is used in many over-the-counter moisturizers and other topical products. Effective topical retinoids have been in use over 30 years but are available only on prescription so are not as widely used as the other topical treatments. Topical retinoids often cause an initial flare up of acne and facial flushing.
Oral retinoids
Main article: isotretinoin
A daily oral intake of vitamin A derivative isotretinoin (marketed as Accutane, Amnesteem, Sotret, Claravis, Clarus) over a period of 4–6 months can cause long-term resolution or reduction of acne. It is believed that isotretinoin works primarily by reducing the secretion of oils from the glands, however some studies suggest that it affects other acne-related factors as well. Isotretinoin has been shown to be very effective in treating severe acne and can either improve or clear well over 80% of patients. The drug has a much longer effect than anti-bacterial treatments and will often cure acne for good. The treatment requires close medical supervision by a dermatologist because the drug has many known side effects (many of which can be severe). About 25% of patients may relapse after one treatment. In those cases, a second treatment for another 4–6 months may be indicated to obtain desired results. It is often recommended that one lets a few months pass between the two treatments, because the condition can actually improve somewhat in the time after stopping the treatment and waiting a few months also gives the body a chance to recover. Occasionally a third or even a fourth course is used, but the benefits are often less substantial. The most common side effects are dry skin and occasional nosebleeds (secondary to dry nasal mucosa). Oral retinoids also often cause an initial flare up of acne within a month or so, which can be severe. There are reports that the drug has damaged the liver of patients. For this reason, it is recommended that patients have blood samples taken and examined before and during treatment. In some cases, treatment is terminated or reduced due to elevated liver enzymes in the blood, which might be related to liver damage. Others claim that the reports of permanent damage to the liver are unsubstantiated, and routine testing is considered unnecessary by some dermatologists. Blood triglycerides also need to be monitored. However, routine testing are part of the official guidelines for the use of the drug in many countries. Some press reports suggest that isotretinoin may cause depression but as of September 2005 there is no agreement in the medical literature as to the risk. The drug also causes birth defects if women become pregnant while taking it or take it while pregnant. For this reason, female patients are required to use two separate forms of birth control or vow abstinence while on the drug. Because of this, the drug is supposed to be given to females as a last resort after milder treatments have proven insufficient. Restrictive rules (see iPledge program) for use were put into force in the USA beginning in March 2006 to prevent misuse, causing occasioned widespread editorial comment.[47]
Phototherapy
Blue' and red light
It has long been known that short term improvement can be achieved with light. Recently, visible light has been successfully employed to treat acne (phototherapy) - in particular intense violet light (405-420 nm) generated by purpose-built fluorescent lighting, dichroic bulbs, LEDslasers. Used twice weekly, this has been shown to reduce the number of acne lesions by about 64%;[48] and is even more effective when applied daily. The mechanism appears to be that a porphyrin (Coproporphyrin III) produced within P. acnes generates free radicals when irradiated by 420 nm and shorter wavelengths of light.[49] Particularly when applied over several days, these free radicals ultimately kill the bacteria.[50] Since porphyrins are not otherwise present in skin, and no UV light is employed, it appears to be safe, and has been licensed by the U.S. FDA.[51] The treatment apparently works even better if used with a mixture of the violet light and red visible light (660 nanometer) resulting in a 76% reduction of lesions after 3 months of daily treatment for 80% of the patients;[52] and overall clearance was similar or better than benzoyl peroxide. Unlike most of the other treatments few if any negative side effects are typically experienced, and the development of bacterial resistance to the treatment seems very unlikely. After treatment, clearance can be longer lived than is typical with topical or oral antibiotic treatments; several months is not uncommon. The equipment or treatment, however, is relatively new and reasonably expensive to buy initially, although the total cost of ownership can be similar to many other treatment methods (such as the total cost of benzoyl peroxide, moisturizer, washes) over a couple of years of use. or
Photodynamic therapy
In addition, basic science and clinical work by dermatologists Yoram Harth and Alan Shalita and others has produced evidence that intense blue/violet light (405-425 nanometer) can decrease the number of inflammatory acne lesion by 60-70% in 4 weeks of therapy, particularly when the P. acnes is pretreated with delta-aminolevulinic acid (ALA), which increases the production of porphyrins. However this photodynamic therapy is controversial and apparently not published in a peer reviewed journal. A phase II trial, while it showed improvement occurred, failed to show improved response compared to the blue/violet light alone.[53]
Laser treatment
Laser surgery has been in use for some time to reduce the scars left behind by acne, but research has been done on lasers for prevention of acne formation itself. The laser is used to produce one of the following effects:
- to burn away the follicle sac from which the hair grows
- to burn away the sebaceous gland which produces the oil
- to induce formation of oxygen in the bacteria, killing them
Since lasers and intense pulsed light sources cause thermal damage to the skin, there are concerns that laser or intense pulsed light treatments for acne will induce hyperpigmented macules (spots) or cause long-term dryness of the skin.
In the United States, the FDA has approved several companies, such as Candela Corp., to use a cosmetic laser for the treatment of acne. However, efficacy studies have used very small sample sizes (fewer than 100 subjects) for periods of six months or less, and have shown contradictory results.[54] Also, laser treatment being relatively new, protocols remain subject to experimentation and revision,[55] and treatment can be quite expensive. Also, some Smoothbeam laser devices had to be recalled due to coolant failure, which resulted in painful burn injuries to patients.[56]
Less widely used treatments
- Aloe vera: there are treatments for acne mentioned in Ayurveda using herbs such as Aloe vera, Neem, Haldi (Turmeric) and Papaya. There is limited evidence from medical studies on some of these products,[57] although others have been proven effective. Products from Rubia cordifolia, Curcuma longa (commonly known as Turmeric), Hemidesmus indicusAzadirachta indica (Neem) have been shown to have anti-inflammatory effects, but not aloe vera.[58] (known as ananthamoola or anantmula), and
- Azelaic acid (brand names Azelex, Finevin and Skinoren) is suitable for mild, comedonal acne.[59]
- Calendula used in suspension is used as an anti-inflammatory agent[60]
- Cortisone injection into spots, also cortisone pills are sometimes used
- Heat: local heating may be used to kill the bacteria in a developing pimple and so speed healing. [61]
- Naproxen or ibuprofen are used for some moderate acne for their anti-inflammatory effect.
- Nicotinamide, (Vitamin B3) used topically in the form of a gel, has been shown in a 1995 study to be of comparable efficacy to topical clindamycin topical antibiotic used for comparison.[62] Topical nicotinamide is available both on prescription and over-the-counter. The property of topical nicotinamide's benefit in treating acne seems to be its anti-inflammatory nature. It is also purported to result in increased synthesis of collagen, keratin, involucrin and flaggrin and may also according to a cosmetic company be useful for reducing skin hyperpigmentation (acne scars), increased skin moisture and reducing fine wrinkles.[63]
- Tea tree oil (melaleuca oil) dissolved in a carrier (5% strength) has been used with some success, where it is comparable to benzoyl peroxide but without excessive drying, kills P. acnes, and has been shown to be an effective anti-inflammatory in skin infections. [57][64][65]
- Rofecoxib was shown to improve premenstrual acne vulgaris in a placebo controlled study.[66]
- Zinc: Orally administered zinc gluconate has been shown to be effective in the treatment of inflammatory acne, although less so than tetracyclines.[67][68]
- Comedo extraction
- Pantothenic acid, (high dosage Vitamin B5)[69]
- Detoxification is a common method used by alternative medicine practitioners for the treatment of acne, although there have been no studies to prove its success. Detoxification is the process of cleansing the body of toxins commonly caused by the environment, pharmaceutical drugs, food, and cosmetics.
- Vitamin and mineral supplementation[70]
History of some acne treatments
The history of acne reaches back to the dawn of recorded history. In Ancient Egypt, it is recorded that several pharaohs were acne sufferers[citation needed]. From Ancient Greece comes the English word 'acne' (meaning 'point' or 'peak'). Acne treatments are also of considerable antiquity:
- Ancient Rome[citation needed]: bathing in hot, and often sulfurous, mineral water was one of the few available acne treatments. One of the earliest texts to mention skin problems is De Medicina by the Roman writer Celsus.
- 1800s: Nineteenth century dermatologists used sulphur in the treatment of acne. It was believed to dry the skin.
- 1920s: Benzoyl Peroxide is used
- 1930s: Laxatives were used as a cure for what were known as 'chastity pimples'. Radiation also was used.
- 1950s: When antibiotics became available, it was discovered that they had beneficial effects on acne. They were taken orally to begin with. Much of the benefit was not from killing bacteria but from the anti-inflammatory effects of tetracycline and its relatives. Topical antibiotics became available later.
- 1970s: Tretinoin (original Trade Name Retin A) was found effective for acne.[71] This preceded the development of oral isotretinoin (sold as Accutane and Roaccutane) in 1980.[72]
- 1980s: Accutane is introduced in the United States, and later found to be a teratogen, highly likely to cause birth defects if taken during pregnancy. In the United States more than 2,000 women became pregnant while taking the drug between 1982 and 2003, with most pregnancies ending in abortion or miscarriage. About 160 babies with birth defects were born.[73][74]
- 1990s: Laser treatment introduced
- 2000s: Blue/red light therapy
- 2000s: Vitamin and mineral nutraceuticals [75]
Future treatments
A vaccine against inflammatory acne has been tested successfully in mice, but it is not certain that it would work similarly in humans.[76]
A 2007 microbiology article reporting the first genome sequencing of a Propionibacterium acnesbacteriophage (PA6) said this "should greatly enhance the development of a potential bacteriophage therapy to treat acne and therefore overcome the significant problems associated with long-term antibiotic therapy and bacterial resistance."[77]
Talarozole, a retinoic acid metabolism blocking agent, is currently under investigation for acne therapy in combination with tretinoin.
Preferred treatments by types of acne vulgaris